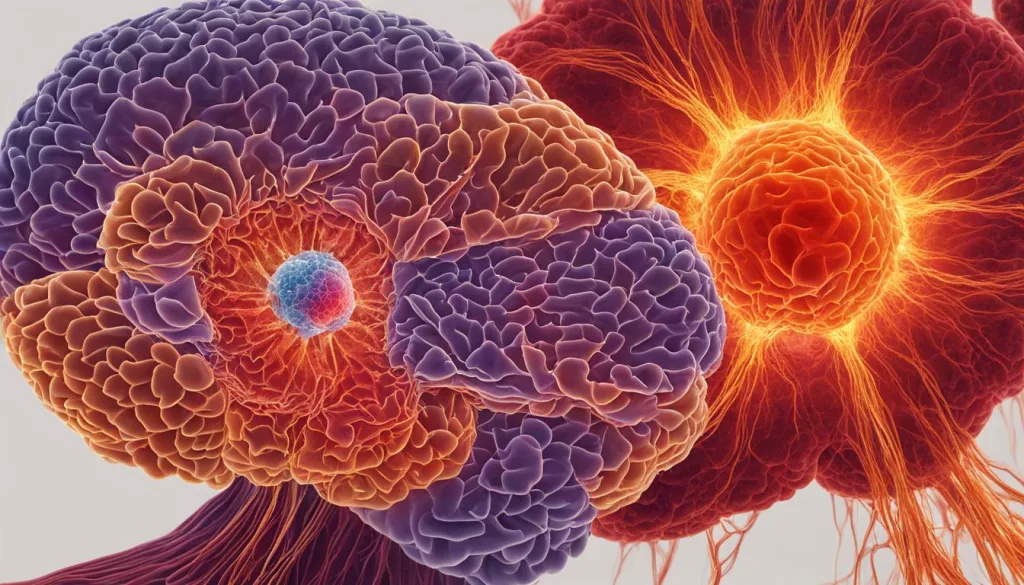
Glioblastoma, a highly aggressive brain tumor, poses significant challenges in terms of treatment and patient outcomes. Current therapies such as surgery, radiotherapy, and chemotherapy have limited effectiveness in combating this deadly disease. However, recent research has shed light on the potential of hyperthermia, a treatment that involves raising the body temperature, to enhance the immune response against glioblastoma.
Hyperthermia has shown promise in selectively damaging tumor cells while sparing healthy cells, making it a compelling approach in cancer treatment. Additionally, hyperthermia has been found to activate the immune system, leading to improved treatment outcomes. By inducing an immune response, hyperthermia can augment the effectiveness of other treatments, such as immunotherapy, radiotherapy, and chemotherapy, thus offering a more comprehensive therapeutic approach.
In this article, we will delve into the role of hyperthermia in enhancing the immune response against glioblastoma, exploring its mechanisms and potential synergies with other treatment modalities. We will also discuss the challenges and future directions in this field of research, as well as the integration of hyperthermia into holistic and non-toxic glioblastoma treatment approaches.
Key Takeaways:
- Hyperthermia, a treatment that increases body temperature, has shown promise in enhancing the immune response against glioblastoma.
- Hyperthermia selectively targets and damages tumor cells while sparing healthy cells, making it a desirable treatment option.
- Immune activation induced by hyperthermia can improve the effectiveness of other treatments like immunotherapy, radiotherapy, and chemotherapy.
- Hyperthermia has been found to selectively kill cancer stem cells, which play a significant role in tumor recurrence and treatment resistance.
- Multiple mechanisms contribute to hyperthermia-induced immune activation, including the release of tumor antigens, activation of dendritic cells, and production of cytokines.
The Role of Hyperthermia in Cancer Treatment
Hyperthermia has been utilized for decades as a valuable modality in cancer treatment. By elevating body temperature, hyperthermia halts the growth of tumor cells and induces apoptosis, or programmed cell death, specifically in cancer cells. The remarkable aspect of hyperthermia is its ability to selectively damage tumor cells while sparing healthy cells, making it an attractive treatment option.
Beyond its direct effects on tumor cells, studies have demonstrated that hyperthermia plays a pivotal role in enhancing the immune response against cancer. This immune activation has been shown to significantly improve treatment outcomes, particularly when hyperthermia is combined with other cancer therapies such as radiotherapy and chemotherapy.
How does hyperthermia bolster the immune response against cancer? Let’s delve deeper into the mechanisms behind this phenomenon.
The Selective Damage of Tumor Cells
When subjected to hyperthermia, tumor cells are exposed to elevated temperatures that surpass their desirable threshold. This thermal stress leads to the destruction of cancer cells through multiple mechanisms:
- Direct cytotoxicity: Hyperthermia can directly induce cellular death by damaging the structural integrity of tumor cells.
- Increased chemosensitivity: By sensitizing tumor cells to chemotherapy, hyperthermia enhances the effectiveness of chemotherapy drugs.
- Radiosensitization: Hyperthermia has been found to sensitize tumor cells to radiation therapy, increasing their vulnerability to radiation-induced damage.
By selectively damaging tumor cells, hyperthermia sets the stage for immune activation, effectively engaging the body’s natural defense mechanism against cancer.
Immune Response Boost and Tumor Microenvironment
Hyperthermia has a profound impact on the tumor microenvironment, triggering an immune response that is instrumental in fighting cancer:
- Promotion of antigen presentation: Hyperthermia aids in the recognition of tumor antigens by immune cells, facilitating the identification and targeting of cancer cells.
- Activation of dendritic cells: Dendritic cells play a crucial role in initiating immune responses by presenting tumor antigens to T cells. Hyperthermia promotes the activation and maturation of dendritic cells, leading to a robust immune response.
- Cytokine release: Hyperthermia triggers the production and release of cytokines, signaling molecules that coordinate and regulate immune responses. These cytokines help recruit and activate immune cells, such as T cells, further bolstering the immune response against cancer.
This orchestration of immune activation within the tumor microenvironment is critical for mounting an effective defense against cancer cells.
Combination Therapies with Hyperthermia
Hyperthermia is often used in conjunction with other cancer treatments to maximize treatment outcomes. Consider the following combination therapies:
| Combination Therapy | Benefits |
|---|---|
| Hyperthermia + Immunotherapy | Enhanced immune response against cancer cells, leading to improved treatment outcomes |
| Hyperthermia + Radiotherapy | Synergistic effects, increasing the effectiveness of radiation therapy and improving tumor control |
| Hyperthermia + Chemotherapy | Increased chemosensitivity of tumor cells, enhancing the efficacy of chemotherapy drugs |
By combining hyperthermia with other therapies, clinicians can optimize treatment approaches and provide comprehensive care to patients.
In the next section, we will delve into the intricate details of the immune response in glioblastoma and explore how hyperthermia can overcome the challenges posed by cancer stem cells.
Immune Response in Glioblastoma
Glioblastoma, a highly aggressive brain tumor, exhibits a complex interaction with the immune system. The tumor microenvironment in glioblastoma creates an immunosuppressive environment, allowing cancer cells to evade the immune response. However, hyperthermia has shown potential in overcoming this immunosuppression and activating the immune system against the tumor.
By inducing an immune response, hyperthermia can enhance the effectiveness of immunotherapy, which utilizes the body’s immune system to target and destroy cancer cells. This immune activation is crucial in improving the outcomes of glioblastoma treatment.
Understanding the Tumor Microenvironment
Glioblastoma fosters an immunosuppressive tumor microenvironment that hinders the immune system’s ability to recognize and eliminate cancer cells. This microenvironment consists of various immunosuppressive factors, such as immune checkpoints and regulatory T cells, that impair immune cell function.
Moreover, cancer cells in glioblastoma actively manipulate the immune response to their advantage, promoting tumor growth and metastasis. These mechanisms make glioblastoma resistant to the body’s natural defense mechanisms.
Hyperthermia’s Impact on the Immune System
Hyperthermia, a treatment that raises body temperature, has been found to enhance the immune response against glioblastoma. By increasing body heat, hyperthermia disrupts the immunosuppressive tumor microenvironment and activates the immune system to target cancer cells.
The hyperthermia-induced immune activation includes the recruitment of immune cells, such as T cells and natural killer cells, to the tumor site. These cells recognize and attack cancer cells, contributing to tumor regression. Additionally, hyperthermia stimulates the production of immune-stimulating cytokines, further boosting the immune response.
Research has shown that combining hyperthermia with immunotherapy can have synergistic effects, promoting a more robust immune response and improving treatment outcomes.
Aiding Immunotherapy with Hyperthermia
Immunotherapy, a cutting-edge cancer treatment, harnesses the power of the immune system to fight cancer. However, glioblastoma’s immunosuppressive environment often limits the effectiveness of immunotherapeutic agents.
Hyperthermia offers a potential solution by activating the immune system and overcoming immunosuppression. This immune activation can help overcome the immune barriers present in glioblastoma and enhance the efficacy of immunotherapy.
By combining hyperthermia with immunotherapy, the immune response can be potentiated, leading to improved tumor targeting and destruction.
Cancer Stem Cells and Hyperthermia
Glioblastoma is a challenging brain tumor characterized by its aggressive nature and high recurrence rates. Within glioblastoma, a subpopulation of cells called cancer stem cells (CSCs) or tumor-initiating cells has been identified. These CSCs are thought to play a crucial role in tumor growth, progression, and treatment resistance. Unlike other cancer cells, CSCs are resistant to conventional therapies, contributing to the regrowth of the tumor and limiting treatment effectiveness.
However, emerging research has shown that hyperthermia, a treatment that increases body temperature, can selectively target and kill these CSCs, disrupting their ability to regrow and contribute to tumor recurrence. Hyperthermia works by leveraging the differential stress response between CSCs and non-CSCs, leading to the preferential elimination of CSCs while sparing normal cells. This targeted approach to eradicating CSCs holds immense promise in enhancing the efficacy of glioblastoma treatment.
By combining hyperthermia with other therapies such as radiotherapy, chemotherapy, or immunotherapy, treatment outcomes for glioblastoma patients can be greatly improved. Hyperthermia provides an additional tool in the fight against cancer, specifically targeting CSCs that are often resistant to other treatments. This integrated approach allows for the comprehensive eradication of both CSCs and non-CSCs, inhibiting tumor growth and increasing the chances of long-term remission.
Benefits of Hyperthermia in Glioblastoma Treatment
Hyperthermia offers several key benefits in the treatment of glioblastoma:
- Selective targeting of CSCs: Hyperthermia can specifically target and eliminate CSCs, disrupting their ability to contribute to tumor growth and recurrence.
- Enhanced treatment efficacy: By combining hyperthermia with other therapies, the overall effectiveness of treatment can be significantly improved. Hyperthermia prepares the terrain by reducing the CSC population, leading to increased susceptibility to radiation, chemotherapy, or immunotherapeutic interventions.
- Reduced treatment resistance: CSCs are often associated with treatment resistance and tumor recurrence. By eliminating these stem-like cells, hyperthermia reduces the chances of treatment resistance and enhances long-term remission rates.
By specifically targeting and eliminating CSCs, hyperthermia plays a crucial role in improving treatment outcomes and prolonging survival for patients with glioblastoma. The integration of hyperthermia with other therapies represents a significant advancement in the fight against this devastating disease.
Table: Comparison of Hyperthermia and Conventional Therapies for Targeting CSCs in Glioblastoma
| Therapy | Selectivity Towards CSCs | Effectiveness against Non-CSC Glioblastoma Cells | Effect on Treatment Resistance |
|---|---|---|---|
| Hyperthermia | High | Selective targeting | Reduced treatment resistance |
| Radiotherapy | Low | Non-selective | Potential treatment resistance |
| Chemotherapy | Variable | Non-selective | Potential treatment resistance |
| Immunotherapy | Variable | Non-selective | Potential treatment resistance |
Mechanisms of Hyperthermia-Induced Immune Activation
Hyperthermia-induced immune activation in glioblastoma involves multiple mechanisms. When the temperature is increased, tumor antigens are released, stimulating the immune system to recognize and target cancer cells. This immune recognition is crucial for effectively eliminating the tumor. Additionally, hyperthermia promotes the activation and maturation of dendritic cells, which play a vital role in initiating immune responses. Dendritic cells capture tumor antigens and present them to T cells, specialized immune cells that can recognize and destroy cancer cells.
Furthermore, hyperthermia can stimulate the production and release of cytokines, signaling molecules that regulate the immune response. These cytokines can enhance the immune activation by attracting immune cells to the tumor site and promoting a pro-inflammatory environment. The combination of these mechanisms works synergistically to enhance the immune response against glioblastoma.

| Mechanism | Description |
|---|---|
| Release of Tumor Antigens | Increased temperature leads to the release of tumor antigens, stimulating immune recognition and targeting of cancer cells. |
| Activation of Dendritic Cells | Hyperthermia promotes the activation and maturation of dendritic cells, which play a crucial role in initiating immune responses by presenting tumor antigens to T cells. |
| Stimulation of Cytokine Production | Hyperthermia stimulates the production and release of cytokines, which regulate the immune response and enhance immune activation. |
These mechanisms highlight the complex and dynamic nature of hyperthermia-induced immune activation in glioblastoma. By understanding these processes, researchers can explore innovative approaches to further enhance the immune response and improve treatment outcomes for patients.
Preclinical and Clinical Studies on Hyperthermia and Glioblastoma
Hyperthermia has shown promise in the treatment of glioblastoma through preclinical and clinical studies. These studies have provided important insights into the effectiveness of hyperthermia in selectively targeting cancer cells, inducing an immune response, and improving treatment outcomes.
Preclinical Studies
Preclinical studies on hyperthermia and glioblastoma have demonstrated encouraging results. These studies involve laboratory experiments and animal models, and they play a critical role in evaluating the potential of new treatments before they are tested in humans.
In preclinical studies, researchers have observed that hyperthermia selectively targets and kills cancer cells in glioblastoma. By increasing the body temperature, hyperthermia damages tumor cells while sparing healthy cells, making it an attractive treatment option.
Furthermore, hyperthermia has been found to induce an immune response in the tumor microenvironment. This immune activation is crucial for enhancing the effectiveness of other treatment modalities, such as immunotherapy, radiotherapy, and chemotherapy.
A significant advantage of hyperthermia in preclinical studies is its ability to target cancer stem cells (CSCs) or tumor-initiating cells. CSCs are resistant to conventional therapies and play a role in tumor recurrence and treatment resistance. Hyperthermia has shown promising results in selectively targeting and killing CSCs, potentially disrupting the tumor’s ability to grow and regenerate.
Clinical Studies
Clinical studies have further demonstrated the potential of hyperthermia in glioblastoma treatment.
These studies involve human subjects and are designed to evaluate the safety, tolerability, and efficacy of hyperthermia as a treatment option.
Clinical studies have shown that hyperthermia is well-tolerated in glioblastoma patients, with minimal side effects. This is an important consideration when exploring new treatment options, as patient safety and quality of life are of utmost importance.
Moreover, clinical studies have indicated improved survival rates in patients receiving hyperthermia as part of their treatment regimen. By activating the immune response and enhancing the effectiveness of other therapies, hyperthermia has the potential to improve treatment outcomes and prolong patient survival.
The findings from preclinical and clinical studies on hyperthermia and glioblastoma suggest that this treatment modality could be a valuable addition to the standard treatment approach. While further research is needed, the promising results thus far highlight the potential of hyperthermia in enhancing immune activation and improving treatment outcomes for glioblastoma patients.
Combination Therapies with Hyperthermia
Hyperthermia, when combined with other treatment modalities, such as immunotherapy, radiotherapy, and chemotherapy, can significantly improve treatment outcomes in patients with glioblastoma multiforme. By leveraging the benefits of different therapies, we can enhance the efficacy of cancer treatments and potentially achieve better control of the tumor.
Hyperthermia and Immunotherapy
Combining hyperthermia with immunotherapy can synergistically potentiate the immune response against glioblastoma. Hyperthermia-induced immune activation primes the immune system to recognize and target cancer cells more effectively, while immunotherapeutic agents enhance the immune response even further. This combination approach holds great promise in improving the outcomes of glioblastoma treatment.
Hyperthermia and Radiotherapy/Chemotherapy
Hyperthermia has also demonstrated synergistic effects with radiotherapy and chemotherapy. By subjecting cancer cells to hyperthermia, their sensitivity to radiotherapy and chemotherapy is increased. This allows for a more effective destruction of tumor cells and a higher likelihood of treatment success.
Overall, the combination of hyperthermia with other treatments offers a comprehensive and multi-pronged approach to glioblastoma treatment. By capitalizing on the unique benefits of each modality, we can optimize treatment outcomes and improve the prospects of patients with this challenging form of cancer.
Challenges and Future Directions in Hyperthermia Research
Despite the promising results of hyperthermia in glioblastoma treatment, there are still challenges that need to be addressed. One of the key challenges is optimizing the treatment parameters of hyperthermia, including temperature, duration, and delivery method. These factors play a crucial role in ensuring the therapeutic efficacy of hyperthermia while minimizing potential side effects.
Another challenge in hyperthermia research is identifying and selecting the right patients for this treatment. Glioblastoma is a heterogeneous disease, and not all patients may benefit equally from hyperthermia. It is essential to identify predictive biomarkers or other factors that can help determine which patients are most likely to respond positively to hyperthermia treatment.
In addition to addressing these challenges, future directions in hyperthermia research include conducting large-scale clinical trials to evaluate the efficacy of hyperthermia in combination with other therapies. This will help us understand the synergistic effects of hyperthermia when used in conjunction with immunotherapy, radiotherapy, or chemotherapy, leading to more effective treatment strategies.
Furthermore, there is a need to refine the treatment protocols for hyperthermia to maximize patient outcomes. This includes determining the optimal treatment schedule, frequency, and duration based on scientific evidence and patient response. By continuously improving the treatment protocols, we can enhance the therapeutic benefits of hyperthermia in glioblastoma.
- Optimizing treatment parameters, including temperature, duration, and delivery method
- Selecting the right patients for hyperthermia treatment
- Conducting large-scale clinical trials to evaluate efficacy in combination therapies
- Refining treatment protocols to maximize patient outcomes
Integrative Approaches in Glioblastoma Treatment
Glioblastoma is a complex and aggressive brain tumor that requires a comprehensive and multidimensional treatment approach. At Brio-Medical Cancer Clinic, we offer integrative oncology programs that combine various therapies to address the unique challenges of glioblastoma.
Our integrative approaches emphasize holistic therapies that aim to support the body’s natural healing abilities while minimizing the use of toxic treatments. We understand the importance of providing non-toxic and natural treatments that not only target the tumor but also promote overall well-being.
One of the key components of our integrative approach is hyperthermia, a treatment that uses heat to selectively target and damage tumor cells. By increasing body temperature, hyperthermia can enhance the immune response against glioblastoma, activating the body’s natural defense mechanisms to fight cancer.
In addition to hyperthermia, we incorporate immunotherapy into our treatment plans. Immunotherapy harnesses the power of the immune system to recognize and destroy cancer cells. By combining hyperthermia with immunotherapy, we aim to amplify the immune response against glioblastoma, improving treatment outcomes and reducing the risk of recurrence.
Our integrative therapies also include natural treatments that complement conventional approaches. These may include nutritional support, supplementation, herbal remedies, and mind-body therapies. By addressing the physical, emotional, and spiritual aspects of healing, we strive to provide a comprehensive treatment approach that supports the whole person.
Benefits of Integrative Approaches:
- Enhanced immune response against glioblastoma
- Selective targeting of tumor cells with hyperthermia
- Reduced toxicity compared to conventional treatments
- Promotion of overall well-being and quality of life
- Complementary support for conventional therapies
Brio-Medical Cancer Clinic: Your Partner in Glioblastoma Treatment
Our team at Brio-Medical Cancer Clinic is dedicated to providing cutting-edge and personalized treatment options for glioblastoma patients. We believe in the power of integrative medicine to optimize treatment outcomes and improve the overall quality of life.
With a focus on non-toxic and holistic therapies, we strive to offer a comprehensive treatment approach that addresses the unique needs of each individual. Our commitment to excellence and patient-centered care sets us apart as a leader in the field of integrative oncology.
Discover the possibilities of integrative approaches in glioblastoma treatment at Brio-Medical Cancer Clinic. Contact us today to learn more about our services and how we can support your journey towards healing and recovery.
Conclusion
We have seen that hyperthermia holds great potential as an effective treatment for glioblastoma, a highly aggressive and recurrent brain tumor. By leveraging its ability to selectively target cancer cells and activate the immune system, hyperthermia can enhance treatment outcomes and potentially reduce tumor recurrence rates. The immune activation induced by hyperthermia can also synergize with other therapies such as immunotherapy, radiotherapy, and chemotherapy, enhancing their effectiveness in fighting glioblastoma.
However, it is important to acknowledge that there are still challenges that need to be addressed in hyperthermia research. We need to optimize treatment parameters and identify the patients who would benefit the most from hyperthermia treatment. Further research and large-scale clinical trials are essential to evaluate the efficacy of hyperthermia in combination with other therapies and refine treatment protocols.
Nevertheless, hyperthermia represents a promising avenue for improving glioblastoma treatment. Its ability to selectively target tumor cells, activate the immune response, and enhance the effectiveness of other treatments make it a valuable addition to the standard treatment for glioblastoma. With continued research and development, hyperthermia has the potential to revolutionize the way we approach and treat this devastating disease.
FAQ
What is hyperthermia in cancer treatment?
Hyperthermia is a treatment that involves increasing the body temperature to selectively damage tumor cells. It can enhance the effectiveness of other therapies, such as radiotherapy and chemotherapy.
How does hyperthermia activate the immune response against glioblastoma?
Hyperthermia induces an immune response by releasing tumor antigens, activating dendritic cells, recruiting and activating T cells, and stimulating the production of cytokines. This immune activation helps the immune system target and destroy cancer cells.
What is the role of hyperthermia in treating cancer stem cells?
Hyperthermia selectively targets and kills cancer stem cells, which are resistant to conventional therapies and contribute to tumor growth and progression. By targeting these cells, hyperthermia can improve treatment outcomes.
How do preclinical and clinical studies support the use of hyperthermia in glioblastoma treatment?
Preclinical studies have demonstrated that hyperthermia selectively targets and kills cancer cells, inducing an immune response and improving treatment outcomes. Clinical studies have shown that hyperthermia is well-tolerated and leads to improved survival rates in glioblastoma patients.
Can hyperthermia be combined with other treatments?
Yes, hyperthermia can be combined with immunotherapy, radiotherapy, and chemotherapy to enhance treatment outcomes. It potentiates the immune response, synergizes with other therapies, and improves control of the tumor.
What are the challenges in using hyperthermia for glioblastoma treatment?
Optimizing treatment parameters and selecting the right patients for hyperthermia are challenges. Further research, including large-scale clinical trials, is needed to evaluate its efficacy and refine treatment protocols.
What are integrative approaches in glioblastoma treatment?
Integrative approaches combine hyperthermia with immunotherapy, natural therapies, and non-toxic treatments to provide comprehensive and holistic treatment for glioblastoma. Brio-Medical Cancer Clinic offers such integrative oncology programs.
What is the potential of hyperthermia in improving glioblastoma treatment?
Hyperthermia can selectively target cancer cells, activate the immune response, and enhance the efficacy of other therapies. It shows promise in reducing tumor recurrence and improving patient outcomes in glioblastoma treatment.




