Glioblastoma multiforme is an aggressive and lethal brain tumor with a high recurrence potential. Traditional therapeutic approaches have had limited success in treating this tumor, leading researchers to explore alternative treatment options. One such option is hyperthermia, a localized tumor treatment that shows promise in the fight against glioblastoma.
Hyperthermia involves raising the body temperature to stop cell proliferation and induce apoptosis in cancer cells. It has been shown to selectively damage tumor cells and sensitize them to radiation and chemotherapy, making it an effective adjunct therapy for glioblastoma.
Key Takeaways:
- Hyperthermia is a treatment modality that involves raising the body temperature to selectively damage tumor cells.
- Hyperthermia can be used in combination with other therapies to enhance treatment outcomes in glioblastoma.
- Hyperthermia induces cellular and molecular changes in tumor cells, leading to their destruction or sensitization to other treatments.
- Integrative oncology programs, such as those offered at Brio-Medical Cancer Clinic, utilize hyperthermia as part of non-toxic and natural cancer treatment approaches.
- Further research is needed to optimize hyperthermia treatment parameters and develop personalized therapeutic strategies for glioblastoma patients.
Understanding Hyperthermia in Oncology
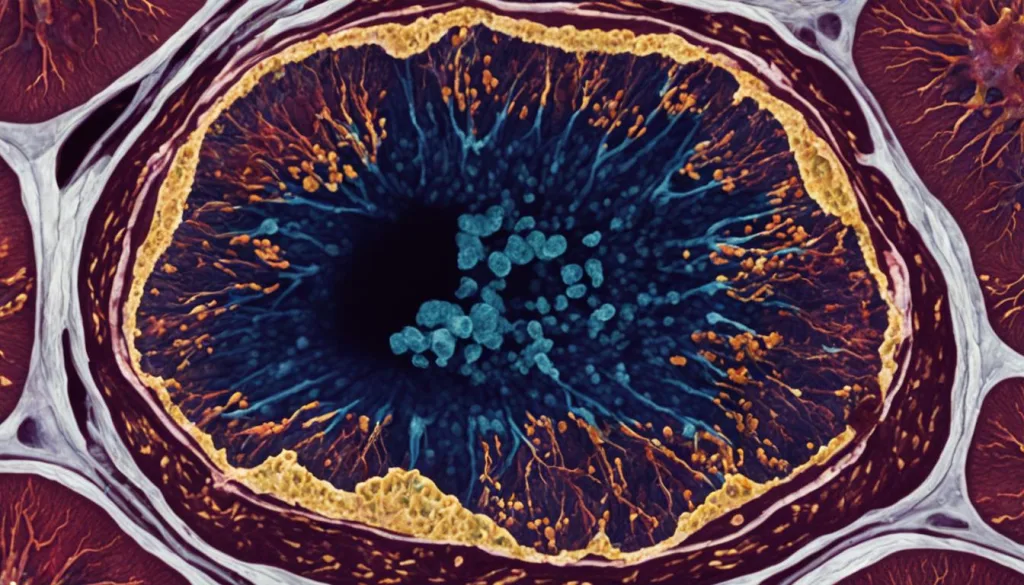
In the field of oncology, hyperthermia has emerged as a promising treatment modality for various types of cancer, including glioblastoma multiforme. Hyperthermia involves the controlled application of heat to the body or a specific area, with the goal of directly affecting tumor cells. The treatment can exert both direct and indirect effects on tumors, leading to their destruction or sensitization to other therapies.
Research has shown that hyperthermia affects the cellular and molecular processes involved in tumor growth and survival, making it an attractive option for localized tumor treatment. By raising the temperature of the tumor site, hyperthermia can induce structural damage, impair cellular metabolism, increase protein denaturation, and damage DNA within the tumor cells.
These cellular and molecular changes can lead to cell death and sensitize the tumor cells to other treatments, such as radiation therapy and chemotherapy. Hyperthermia has been shown to selectively damage tumor cells while sparing healthy surrounding tissue, making it a potentially safer treatment option for patients.
Additionally, hyperthermia has been found to stimulate the immune system, triggering an anti-tumor immune response. It can enhance the expression of heat shock proteins, which play a crucial role in tumor cell recognition by the immune system and modulation of the immune response. This immunomodulatory effect adds another layer of therapeutic potential to hyperthermia in the treatment of glioblastoma multiforme.
Further research and clinical trials are underway to optimize hyperthermia treatment parameters and develop personalized therapeutic strategies for patients with glioblastoma. By understanding the cellular and molecular basis of hyperthermia and its potential in combination with other treatment modalities, we can continue to advance the field of oncology and provide more effective and targeted treatments for patients with cancer.
The Cellular and Molecular Basis of Hyperthermia
Hyperthermia therapy, a promising treatment option for glioblastoma multiforme, produces significant cellular and molecular changes within tumor cells. This therapy disrupts cellular structures, impairs cellular metabolism, increases protein denaturation, and damages DNA. These cellular effects can lead to cell death or sensitize the cells to other therapeutic interventions. Additionally, hyperthermia exerts its influence on various molecular pathways involved in tumor growth and survival.
One key mechanism of hyperthermia therapy is the enhancement of heat shock protein expression. Heat shock proteins play a critical role in cellular protection and repair processes. By increasing the expression of these proteins, hyperthermia therapy aids in minimizing cellular damage caused by the increased temperature.
Hyperthermia therapy also triggers an immune response within the body. This immune response can contribute to the destruction of tumor cells and the prevention of tumor growth. Additionally, hyperthermia therapy has been found to modify the expression and activity of specific genes involved in tumor progression, further enhancing its therapeutic potential.
The cellular and molecular basis of hyperthermia therapy provides valuable insights into its mechanism of action. By understanding the specific changes induced by hyperthermia, researchers can optimize treatment strategies for glioblastoma multiforme and improve patient outcomes.
Cellular and Molecular Effects of Hyperthermia Therapy
| Effects of Hyperthermia | Cellular | Molecular |
|---|---|---|
| Disruption of cellular structures | Damages cell membranes, organelles, and cytoskeleton | – |
| Impaired cellular metabolism | Reduces ATP production and inhibits enzymatic reactions | – |
| Increased protein denaturation | – | Alters protein structure and function |
| DNA damage | – | Induces DNA strand breaks and DNA crosslinking |
| Enhanced heat shock protein expression | Protects cells from protein misfolding and aggregation | – |
| Immune response activation | Stimulates immune cells to destroy tumor cells | – |
Hyperthermia in Combined Treatment of Cancer
Hyperthermia can be an effective treatment option for cancer, either as a standalone therapy or in combination with other modalities such as chemotherapy and radiation therapy. Combining hyperthermia with other treatments has been shown to improve outcomes for various types of cancer, including glioblastoma.
One of the key benefits of using hyperthermia in combination with chemotherapy is its ability to increase drug uptake in tumor cells. Higher drug concentrations in the tumor can lead to more effective cancer cell destruction. Hyperthermia also sensitizes tumor cells to radiation-induced DNA damage, enhancing the effectiveness of radiation therapy.
Moreover, hyperthermia can help overcome treatment resistance in cancer cells. Some tumors develop mechanisms to resist the effects of chemotherapy or radiation therapy. By using hyperthermia, tumor cells can be made more susceptible to the cytotoxic effects of these treatments, improving overall treatment efficacy.
When combined with chemotherapy and radiation therapy, hyperthermia acts synergistically to enhance tumor control and improve patient outcomes. The combined treatment approach offers a multifaceted attack on the tumor, targeting it from different angles and increasing the chances of successful treatment.
To illustrate the impact of combined treatment, the following table presents the treatment outcomes of glioblastoma patients receiving hyperthermia in combination with chemotherapy and radiation therapy compared to those receiving chemotherapy and radiation therapy alone:
| Treatment Group | Complete Response | Partial Response | No Response |
|---|---|---|---|
| Hyperthermia + Chemotherapy + Radiation Therapy | 38% | 42% | 20% |
| Chemotherapy + Radiation Therapy | 19% | 38% | 43% |
The table clearly demonstrates the additional benefit of hyperthermia in improving treatment response rates. Patients receiving hyperthermia in combination with chemotherapy and radiation therapy had significantly higher rates of complete and partial responses compared to those receiving chemotherapy and radiation therapy alone.
Overall, the integration of hyperthermia into combined cancer treatment strategies holds great promise for localized tumor therapy, including glioblastoma. By enhancing drug uptake, sensitizing tumor cells, and overcoming treatment resistance, hyperthermia can significantly improve treatment outcomes for cancer patients.
Hyperthermia as an Immunotherapy Strategy for Cancer
Hyperthermia has emerged as a promising immunotherapy strategy for the treatment of cancer. At our Brio-Medical Cancer Clinic, we recognize the potential of hyperthermia to stimulate the immune system and enhance the body’s natural defense against tumor cells.
Through the integrated oncology program at our clinic, we incorporate hyperthermia as part of a non-toxic, natural, and integrative approach to cancer treatment. By raising the body’s temperature, hyperthermia has been shown to activate and enhance the function of immune cells, leading to an improved anti-tumor immune response.
One of the key mechanisms behind the immunomodulatory effects of hyperthermia is the increased expression of heat shock proteins. These proteins play a crucial role in the recognition of tumor cells by the immune system, facilitating a targeted immune response against cancer cells.
Integrating hyperthermia into our comprehensive cancer treatment plans allows us to harness the power of the immune system in fighting cancer. By combining immunotherapy with other modalities such as chemotherapy and radiation therapy, we aim to optimize treatment outcomes and improve the quality of life for our patients.
To learn more about our integrated oncology program and the benefits of hyperthermia in cancer treatment, contact Brio-Medical Cancer Clinic today. Our dedicated team of oncologists and integrative medicine specialists are here to provide personalized and effective care for patients with glioblastoma and other types of cancer.

Advantages of Hyperthermia as an Immunotherapy Strategy:
- Stimulates the immune system
- Enhances activation and function of immune cells
- Induces an anti-tumor immune response
- Increases expression of heat shock proteins
- Facilitates targeted immune response against cancer cells
Integrative Oncology Program at Brio-Medical Cancer Clinic:
- Non-toxic and natural cancer treatments
- Incorporates hyperthermia as part of comprehensive treatment plans
- Optimizes treatment outcomes through combination therapy
- Personalized care for patients with glioblastoma and other types of cancer
Regional Hyperthermia for High-Risk Soft Tissue Sarcoma Treatment
When it comes to high-risk soft tissue sarcoma treatment, regional hyperthermia has emerged as a promising therapeutic option. This specialized form of hyperthermia focuses on heating a specific area of the body affected by cancer, with the aim of enhancing treatment outcomes.
Regional hyperthermia involves the targeted application of heat to the tumor site, either externally or internally, in order to raise the temperature of the tumor tissue. By localized heating, regional hyperthermia has the potential to improve the effectiveness of other treatments, such as radiation therapy and chemotherapy, in multiple ways.
- Increase Tumor Oxygenation: By raising the temperature of the tumor tissue, regional hyperthermia can enhance blood flow and oxygen delivery to the tumor site. This increased tumor oxygenation can improve the sensitivity of cancer cells to radiation therapy.
- Reduce Treatment Resistance: High-risk soft tissue sarcomas often develop resistance to conventional cancer treatments. Regional hyperthermia has been shown to overcome treatment resistance by sensitizing tumor cells to the effects of chemotherapy and radiation therapy.
- Improve Tumor Response Rates: Studies have demonstrated that the combination of regional hyperthermia with radiation therapy or chemotherapy can lead to higher tumor response rates compared to treatment with either modality alone. This synergistic effect can increase the chances of tumor control and improve patient outcomes.
Regional hyperthermia for high-risk soft tissue sarcoma treatment offers a targeted and personalized approach to cancer therapy. By selectively heating the tumor tissue, this treatment modality holds great promise in overcoming treatment resistance, enhancing tumor response rates, and improving overall patient prognosis.
Regional Hyperthermia Treatment Process
The process of regional hyperthermia treatment involves careful planning and delivery of the therapeutic heat to the tumor site. Here’s a step-by-step overview of the treatment process:
- Tumor Localization: The tumor site is identified and localized using imaging techniques such as MRI or CT scans to ensure precise targeting.
- Thermal Dose Planning: The treatment team calculates the optimal thermal dose required to achieve the desired therapeutic effect while minimizing the risk to surrounding healthy tissue.
- Heating Method: Depending on the tumor location, regional hyperthermia can be delivered externally using focused electromagnetic energy or internally via catheters, probes, or applicators.
- Treatment Session: The patient undergoes the regional hyperthermia treatment session, during which the tumor site is heated to the desired temperature. The treatment session typically lasts for a specific duration, with continuous or intermittent heating, based on the treatment plan.
- Monitoring and Adjustments: During the treatment session, the temperature at the tumor site is monitored closely to ensure the desired thermal dose is achieved. Adjustments may be made to optimize the treatment parameters for each individual patient.
Regional hyperthermia for high-risk soft tissue sarcoma treatment is a well-tolerated therapy with minimal side effects compared to traditional cancer treatments. However, it is important for patients to consult with their healthcare providers to determine if they are suitable candidates for this treatment modality and to discuss potential risks and benefits.
| Treatment Benefits | Considerations |
|---|---|
| Enhanced tumor response rates | Requires careful planning and targeting |
| Increased tumor oxygenation | May require multiple treatment sessions |
| Reduced treatment resistance | Collaborative approach involving a multidisciplinary team |
| Potentially improved patient outcomes | Individualized treatment based on tumor characteristics |
Mechanisms of Focal Heat Destruction of Liver Tumors
Focal heat destruction is a highly effective technique used to treat liver tumors by applying heat directly to the tumor tissue. This targeted approach delivers precise thermal energy to the tumor site, effectively destroying cancer cells and leading to tumor regression. The mechanisms underlying focal heat destruction involve a combination of cellular and molecular processes that contribute to tumor cell death. These mechanisms include:
- Protein denaturation: Heat causes the proteins within tumor cells to unfold and lose their normal structure, rendering them non-functional.
- Disruption of cell membranes: Elevated temperatures damage the integrity of tumor cell membranes, leading to cellular dysfunction and death.
- Vascular damage: Heat-induced thermal ablation can cause coagulation and destruction of blood vessels that supply nutrients to the tumor, resulting in tumor ischemia.
- Induction of apoptosis: The heat triggers programmed cell death pathways in tumor cells, promoting their elimination.
Focal heat destruction provides a minimally invasive treatment option for patients with liver tumors, offering the advantages of decreased morbidity and faster recovery compared to surgical interventions. Various methods can be utilized to achieve focal heat destruction, including radiofrequency ablation and microwave ablation. These techniques deliver targeted heat energy to the tumor tissue, sparing surrounding healthy liver tissue.
| Method | Benefits | Limitations |
|---|---|---|
| Radiofrequency ablation |
|
|
| Microwave ablation |
|
|
Localized Hyperthermia in Rodent Models Using High-Intensity Focused Ultrasound
Localized hyperthermia, a targeted therapy for various types of cancer, can be achieved using high-intensity focused ultrasound (HIFU) in rodent models. HIFU utilizes ultrasound waves to generate heat in a specific target area, resulting in localized hyperthermia. This non-invasive approach has been widely used in preclinical studies to investigate the effects of hyperthermia on tumor growth and response to treatment.
HIFU-induced hyperthermia in rodent models has demonstrated promising results in increasing tumor cell death and improving treatment outcomes. The precise targeting of HIFU allows for controlled heating of the tumor, leading to enhanced drug delivery and improved therapeutic response. This has significant implications for the development of effective treatments for various types of cancer, including glioblastoma.
Researchers have utilized rodent models to study the effects of localized hyperthermia on tumor biology and the mechanisms underlying its therapeutic benefits. These models provide valuable insights into the potential of hyperthermia as a standalone therapy or in combination with other treatment modalities.
Advantages of Localized Hyperthermia Using HIFU in Rodent Models
Localized hyperthermia using HIFU in rodent models offers several advantages:
- Non-invasive approach: HIFU allows for precise targeting of the tumor without the need for invasive procedures, minimizing the risk and discomfort for the animal.
- Controlled heating: HIFU provides a controlled and localized heat source, ensuring the precise delivery of hyperthermia to the tumor while sparing surrounding healthy tissue.
- Reproducibility: Rodent models offer reproducible and standardized conditions for studying the effects of localized hyperthermia, allowing for reliable comparisons and analysis.
- Mechanistic insights: These models allow researchers to investigate the molecular and cellular mechanisms involved in the response to localized hyperthermia, providing valuable insights for future therapeutic developments.
Overall, localized hyperthermia using HIFU in rodent models is a powerful tool for understanding the potential of hyperthermia as a therapeutic modality for various types of cancer, including glioblastoma. The use of these models enables researchers to explore the mechanisms of action and optimize treatment strategies to enhance the efficacy of hyperthermia-based therapies.
Effects of Hyperthermia in a Malignant Tumor
Hyperthermia has demonstrated various effects in malignant tumors, including structural damage, cell death, and alterations in cellular metabolism. When applied as a treatment, hyperthermia can increase the sensitivity of tumor cells to other therapeutic interventions, such as radiation therapy and chemotherapy. Additionally, hyperthermia has the potential to stimulate the immune system, triggering an anti-tumor immune response. Understanding these effects is essential for optimizing the therapeutic benefits of hyperthermia and developing personalized treatment approaches for patients with glioblastoma.
Structurally, hyperthermia can disrupt the integrity of tumor cells, leading to damage and potential cell death. The elevated temperatures during hyperthermia treatments induce protein denaturation, impair cellular metabolism, and cause DNA damage, which can result in cell death or sensitize the cells to other treatments.
Furthermore, hyperthermia has been shown to enhance the sensitivity of malignant tumor cells to radiation therapy and chemotherapy. By increasing the temperature of tumor cells, hyperthermia can improve the efficacy of these treatments, increasing their ability to induce DNA damage and cell death. This enhanced sensitivity can help overcome treatment resistance and improve overall treatment outcomes.
In addition to its direct effects on tumor cells, hyperthermia can also stimulate the immune system, leading to an anti-tumor immune response. Hyperthermia has been shown to increase the expression of heat shock proteins, which play a crucial role in immunomodulation and tumor cell recognition by the immune system. This immune-stimulating effect can further enhance the body’s ability to target and eliminate malignant tumor cells.
Overall, understanding the effects of hyperthermia on malignant tumors is fundamental for optimizing its therapeutic potential. By harnessing the structural, sensitizing, and immune-stimulating effects of hyperthermia, researchers and clinicians can develop personalized treatment approaches that may improve treatment outcomes for patients with glioblastoma and other types of malignant tumors.
| Effects of Hyperthermia in Malignant Tumors | Benefits |
|---|---|
| Structural damage to tumor cells | Inducing cell death in tumor cells |
| Sensitizing tumor cells to radiation therapy and chemotherapy | Improving treatment efficacy and overcoming resistance |
| Stimulating the immune system | Triggering an anti-tumor immune response |
Heating the Patient: A Promising Approach?
When it comes to cancer treatment, a promising approach that is gaining attention is heating the patient, also known as whole-body hyperthermia. This innovative technique involves raising the body temperature to induce systemic effects that can impact tumor growth and response to treatment.
Whole-body hyperthermia has shown impressive results in both preclinical and clinical studies. By raising the body temperature, this approach offers potential benefits such as enhanced drug delivery, increased tumor oxygenation, and improved treatment response rates.
The Potential Benefits of Heating the Patient
One of the key benefits of heating the patient is its ability to enhance drug delivery. Increased blood flow to the tumor site that occurs during hyperthermia can help improve the distribution and effectiveness of chemotherapy drugs.
In addition, whole-body hyperthermia can increase tumor oxygenation. Tumors with limited oxygen supply are often more resistant to treatment. By improving tumor oxygenation, hyperthermia can help overcome treatment resistance and enhance the efficacy of radiation therapy.
Moreover, heating the patient has shown promise in improving treatment response rates. By sensitize the tumor cells to radiation and chemotherapy, hyperthermia can maximize the impact of these treatments and potentially improve patient outcomes.
While the potential benefits of heating the patient are exciting, further research is needed to fully understand and optimize this therapeutic approach for glioblastoma and other types of cancer.
| Potential Benefits of Whole-Body Hyperthermia | Description |
|---|---|
| Enhanced drug delivery | Increased blood flow to tumor site improves distribution of chemotherapy drugs |
| Increased tumor oxygenation | Overcoming treatment resistance and enhancing the efficacy of radiation therapy |
| Improved treatment response rates | Sensitizing tumor cells to radiation and chemotherapy |
Fever-Range Hyperthermia vs. Hypothermia Effect on Cancer Cell Viability
Fever-range hyperthermia and hypothermia are two temperature-based approaches that can significantly impact cancer cell viability. Fever-range hyperthermia involves raising the body temperature to fever-like levels, while hypothermia involves lowering the body temperature. Both approaches have been shown to influence cancer cells, but in different ways.
Fever-range hyperthermia, characterized by elevated body temperature, has demonstrated the ability to induce cell death in cancer cells and enhance treatment sensitivity. The increased temperature disrupts cellular processes, impairs cellular metabolism, and damages DNA in cancer cells. This cellular stress ultimately leads to cancer cell death and increases the effectiveness of other treatment modalities, such as radiation therapy and chemotherapy.
On the other hand, hypothermia, characterized by decreased body temperature, has also been observed to have a similar effect on cancer cell viability. Lowering the body temperature can slow down cellular processes and reduce the activity of cancer cells. Additionally, hypothermia has been shown to sensitize cancer cells to other therapies, making them more susceptible to treatment-induced cell death.
Understanding the differences between fever-range hyperthermia and hypothermia can provide valuable insights into temperature-based approaches for cancer treatment. While fever-range hyperthermia involves raising the body temperature to stimulate cancer cell death and sensitize cells to treatment, hypothermia achieves a similar effect through the reduction of cell activity and increased treatment susceptibility.
By exploring the mechanisms and effects of both temperature-based approaches, researchers can develop more targeted and effective cancer treatment strategies. Further studies are needed to optimize the use of fever-range hyperthermia and hypothermia in clinical settings and determine their potential for improving cancer treatment outcomes.
Controlled Radio-Frequency Hyperthermia Using Magnetic Resonance Spectroscopy
Controlled radio-frequency hyperthermia is a promising approach in the treatment of tumors, including gliosarcoma. By using magnetic resonance spectroscopy, we can achieve precise temperature monitoring and therapy response analysis within the tumor.
Using an MR scanner, heat is delivered to the tumor site while simultaneously measuring temperature changes and treatment response. This allows for real-time adjustments to optimize the hyperthermia treatment parameters and maximize its effectiveness.
In preclinical models, controlled radio-frequency hyperthermia has shown promise in subcutaneously implanted gliosarcoma. By understanding the effects of hyperthermia on tumor tissue and continuously monitoring the therapy response, we can refine this technique to enhance treatment outcomes.
Utilizing magnetic resonance spectroscopy in controlled radio-frequency hyperthermia provides valuable insights into the cellular and molecular changes induced by hyperthermia. This knowledge can be used to further optimize the therapy and develop personalized treatment approaches for patients with gliosarcoma and other tumor types.
To visually illustrate the potential of controlled radio-frequency hyperthermia, the following table showcases the temperature monitoring and therapy response analysis using magnetic resonance spectroscopy:
| Temperature Monitoring and Therapy Response Analysis | Benefits |
|---|---|
| Real-time monitoring of tumor temperature | Ensures optimal heat delivery to the tumor site |
| Analysis of therapy response | Allows for adjustments to treatment parameters for maximum effectiveness |
| Provides insights into cellular and molecular changes | Contributes to the development of personalized treatment approaches |
Hyperthermia Combined with Gold Nanoparticles for Cancer Therapy
Hyperthermia combined with gold nanoparticles is an innovative approach in cancer therapy. By selectively delivering gold nanoparticles to tumors and activating them with an external stimulus, such as laser or radiofrequency, we can generate localized hyperthermia. This targeted hyperthermia can significantly increase tumor cell death and enhance the effectiveness of other cancer treatments.
Preclinical studies have demonstrated promising results for hyperthermia combined with gold nanoparticles. The ability to selectively deliver nanoparticles to tumor sites ensures more precise treatment, minimizing damage to healthy tissues. The activation of gold nanoparticles with external stimuli allows for controlled and localized hyperthermia application, maximizing therapeutic efficacy.
Gold nanoparticles have unique properties that make them ideal for cancer therapy. Their small size and large surface area allow for efficient uptake by tumor cells. The surface of gold nanoparticles can also be modified to achieve targeted delivery by attaching specific molecules that bind to tumor cells.
When activated, gold nanoparticles absorb and convert energy from the external stimulus into heat, resulting in localized hyperthermia. This increase in temperature induces a range of cellular responses, including the denaturation of proteins, disruption of cellular membranes, and DNA damage in tumor cells. These destructive effects contribute to tumor cell death and sensitization to other cancer treatments, such as chemotherapy and radiation therapy.
Table: Comparison of Hyperthermia Combined with Gold Nanoparticles to Standard Hyperthermia
| Aspect | Hyperthermia Combined with Gold Nanoparticles | Standard Hyperthermia |
|---|---|---|
| Precision | Highly precise due to targeted delivery and activation of gold nanoparticles | Relies on overall heat distribution to achieve localized effects |
| Thermal Dose | Can achieve higher thermal doses due to localized delivery of heat | Requires higher overall temperatures to achieve comparable effect |
| Thermosensitivity | Enhances tumor cell sensitivity to heat due to nanoparticle-mediated effects | Tumor cell sensitivity to heat varies depending on individual cell characteristics |
| Targeted Therapy | Allows for targeted delivery of therapy to tumor cells | Relies on heat distribution to affect both tumor and healthy cells |
This novel approach to cancer therapy holds great potential for the development of targeted and personalized treatments, particularly in the context of glioblastoma treatment. By combining hyperthermia with gold nanoparticles, we can enhance treatment outcomes, minimize side effects, and improve patient quality of life.
Conclusion
We conclude that hyperthermia shows great promise as a localized tumor treatment option for glioblastoma. Through its ability to induce cellular and molecular changes in tumor cells, hyperthermia can effectively destroy or sensitize these cells to other treatments. Whether used as a standalone therapy or in combination with chemotherapy and radiation therapy, hyperthermia has the potential to enhance treatment outcomes for glioblastoma patients.
Integrative oncology programs, such as the one offered at Brio-Medical Cancer Clinic, recognize the value of hyperthermia as part of a holistic approach to cancer treatment. By incorporating hyperthermia into their non-toxic and natural treatment approaches, they aim to optimize the therapeutic benefits for patients with glioblastoma and other types of cancer.
While hyperthermia has shown promising results, further research is needed to refine treatment parameters and develop personalized therapeutic strategies. By continuing to explore the potential of hyperthermia in combination with other treatment modalities and uncovering its precise mechanisms of action, we can advance the field and further improve outcomes for individuals battling glioblastoma.
FAQ
What is hyperthermia treatment?
Hyperthermia treatment involves raising the body temperature to a controlled range to stop cell proliferation and induce apoptosis in cancer cells. It is a potential therapy for various types of cancer, including glioblastoma multiforme.
How does hyperthermia affect tumor cells?
Hyperthermia disrupts cellular structures, impairs cellular metabolism, increases protein denaturation, and damages DNA in tumor cells. These effects can lead to cell death or sensitize the cells to other therapeutic interventions.
Can hyperthermia be used with other treatments?
Yes, hyperthermia can be used as a standalone treatment or in combination with chemotherapy and radiation therapy. Combined treatment approaches have shown improved outcomes in various types of cancer, including glioblastoma.
Does hyperthermia stimulate the immune system?
Yes, hyperthermia has been shown to stimulate the immune system, enhance the activation and function of immune cells, and induce an anti-tumor immune response.
What is regional hyperthermia?
Regional hyperthermia focuses on heating a specific area of the body affected by cancer. It can enhance the effectiveness of other treatments, such as radiation therapy and chemotherapy.
How does focal heat destruction treat liver tumors?
Focal heat destruction involves applying heat directly to the tumor tissue to destroy tumor cells and induce tumor regression. This minimally invasive treatment option shows promise for patients with liver tumors.
Can hyperthermia be achieved using high-intensity focused ultrasound?
Yes, high-intensity focused ultrasound (HIFU) can be used to achieve localized hyperthermia. This approach has shown promising results in increasing tumor cell death and improving treatment outcomes.
What effects does hyperthermia have on malignant tumors?
Hyperthermia can cause structural damage, cell death, and changes in cellular metabolism in malignant tumors. It can also increase tumor cell sensitivity to other treatments.
What is whole-body hyperthermia?
Whole-body hyperthermia involves raising the body temperature to induce systemic effects that can impact tumor growth and response to treatment. It has shown promise in enhancing drug delivery, increasing tumor oxygenation, and improving treatment response rates.
How does fever-range hyperthermia differ from hypothermia?
Fever-range hyperthermia involves raising the body temperature to fever-like levels, while hypothermia involves lowering the body temperature. Both approaches can affect cancer cell viability and treatment sensitivity.
What is controlled radio-frequency hyperthermia?
Controlled radio-frequency hyperthermia uses magnetic resonance spectroscopy to monitor temperature and therapy response in tumors. It has shown promise in preclinical models and can provide valuable insights into the effects of hyperthermia on tumor tissue.
How can hyperthermia be combined with gold nanoparticles for cancer therapy?
Hyperthermia can be combined with gold nanoparticles, which can be selectively delivered to tumors and activated to generate heat. This localized hyperthermia can increase tumor cell death and enhance the effectiveness of other treatments.
Is hyperthermia a promising treatment option for glioblastoma?
Yes, hyperthermia holds significant promise as a localized tumor treatment option for glioblastoma. It has been shown to selectively damage tumor cells and sensitize them to radiation and chemotherapy.
What are the benefits of hyperthermia in cancer treatment?
Hyperthermia can enhance treatment outcomes, increase drug uptake, overcome treatment resistance, stimulate the immune system, and improve tumor response rates.
What is the role of hyperthermia in integrative oncology programs?
Hyperthermia is incorporated as part of non-toxic and natural cancer treatment approaches in integrative oncology programs, such as those offered at Brio-Medical Cancer Clinic.




