Glioblastoma multiforme (GBM) is a highly aggressive and lethal brain tumor with limited treatment options. However, there is hope on the horizon with the potential of hyperthermia to target and reduce the size of GBM tumors. Hyperthermia, a non-invasive treatment approach, has shown promise in inhibiting tumor growth and recurrence, making it a potential therapeutic option for GBM patients.
Key Takeaways:
- Hyperthermia is a non-invasive treatment approach for GBM.
- Hyperthermia has shown promise in reducing tumor size and inhibiting recurrence.
- Various hyperthermia techniques, such as microwaves, radiofrequency, lasers, ultrasound, and magnetic fluid hyperthermia, can be used for GBM treatment.
- Hyperthermia can induce apoptosis, inhibit cell proliferation, and disrupt DNA repair mechanisms in GBM cells.
- Clinical studies have demonstrated the effectiveness of hyperthermia in reducing tumor size and improving patient outcomes in GBM.
Understanding Glioblastoma Multiforme
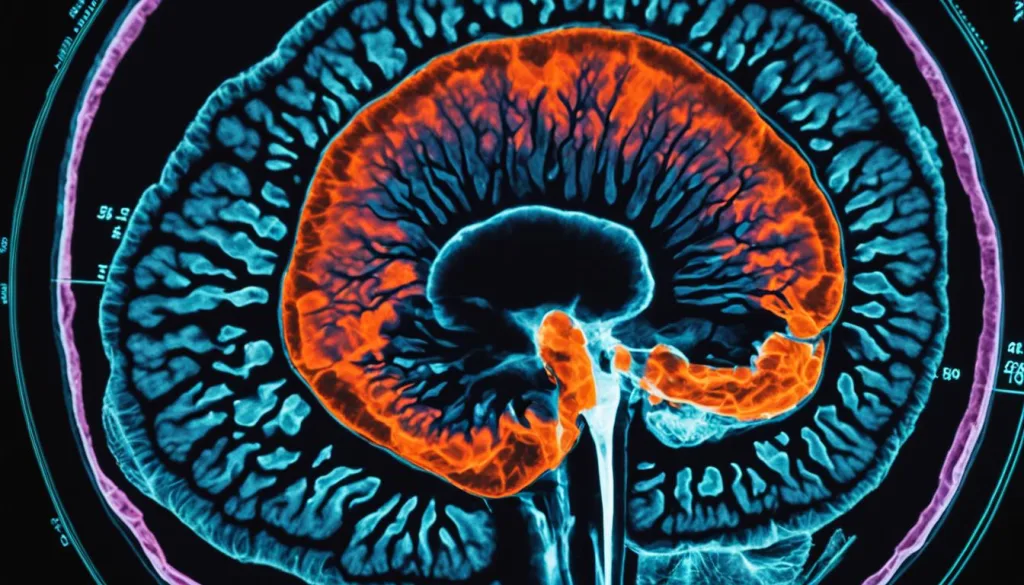
Glioblastoma multiforme (GBM) is an aggressive and lethal brain tumor that poses significant challenges in treatment. Despite current methods such as surgery, radiotherapy, and chemotherapy, GBM has a high recurrence rate, making it one of the most challenging brain tumors to manage. To gain insights into the complex nature of GBM, researchers have explored the cellular and molecular mechanisms underlying its development and progression.
The Role of Cancer Stem-Like Cells
Efforts to understand GBM have led to the identification of cancer stem-like cells (CSCs) within the tumor. These CSCs are a small subpopulation of cells that exhibit self-renewal and differentiation capabilities, playing a pivotal role in tumor growth, recurrence, and treatment resistance. By investigating the characteristics and behavior of CSCs, researchers aim to develop targeted therapies that can specifically eliminate these cells and improve treatment outcomes.
The Challenge of Tumor Recurrence
Tumor recurrence is one of the most pressing issues in GBM treatment. Despite successfully removing the primary tumor, the remaining cancer cells can initiate the formation of new tumors. This recurrence is attributed to the invasive nature of GBM cells, which infiltrate surrounding healthy brain tissue. Identifying the factors that contribute to tumor recurrence and developing strategies to prevent its onset are critical for improving the prognosis of GBM patients.
New Insights into Treatment Resistance
Another significant challenge in GBM treatment is the development of resistance to conventional therapies. GBM cells can acquire resistance mechanisms that allow them to evade the cytotoxic effects of chemotherapy and radiotherapy. Understanding the molecular pathways involved in treatment resistance can aid in the development of targeted therapies that can overcome these mechanisms and enhance treatment efficacy.
Advances in Molecular Profiling
Advances in technology have facilitated molecular profiling of GBM tumors, enabling a deeper understanding of the genetic and molecular alterations that drive tumor progression. This information can guide the development of personalized treatment strategies that target specific genetic mutations or dysregulated pathways.
The Need for Innovative Treatment Approaches
Given the challenges associated with GBM, there is a pressing need for innovative treatment approaches that can improve patient outcomes. Targeted therapies, immunotherapies, and combination treatments are being explored to overcome treatment resistance and enhance the effectiveness of current treatment modalities. Additionally, the role of the tumor microenvironment and its interaction with the immune system is an area of active research.
The Role of Hyperthermia in GBM Treatment
Hyperthermia, a non-invasive treatment approach, plays a significant role in the treatment of glioblastoma multiforme (GBM). By raising the body temperature, hyperthermia selectively targets and damages tumor cells, inducing apoptosis and sensitizing cancer cells to radiotherapy and chemotherapy. This promising therapy has been explored in various forms, including microwaves, radiofrequency, lasers, ultrasound, and magnetic fluid hyperthermia.
Studies have demonstrated the effectiveness of hyperthermia in reducing tumor size, inhibiting recurrence, and improving treatment outcomes in GBM patients. The ability to selectively destroy tumor cells while minimizing damage to healthy tissues makes hyperthermia a valuable therapeutic option.
Hyperthermia Treatment Techniques for GBM
Hyperthermia techniques used in GBM treatment include:
- Microwaves
- Radiofrequency
- Lasers
- Ultrasound
- Magnetic Fluid Hyperthermia
Each technique has its advantages and limitations, and the choice depends on factors such as tumor location, size, and patient suitability. The goal is to raise the temperature in the tumor region, promoting tumor cell death while preserving healthy surrounding tissues.
| Hyperthermia Technique | Advantages | Limitations |
|---|---|---|
| Microwaves | Deep tissue penetration | Requires advanced temperature monitoring |
| Radiofrequency | Precise heat delivery | Device limitations for certain tumor locations |
| Lasers | Localized heat generation | Limited depth of penetration |
| Ultrasound | Real-time temperature monitoring | Dependent on acoustic properties of tissues |
| Magnetic Fluid Hyperthermia | Potential for targeted drug delivery | Requires specialized magnetic nanoparticles |
The choice of hyperthermia technique depends on the specific requirements of each GBM case, aiming to achieve optimal treatment outcomes.
Cellular and Molecular Effects of Hyperthermia on GBM
Hyperthermia, as a non-invasive treatment approach, exerts profound effects on glioblastoma multiforme (GBM) at the cellular and molecular levels. By raising the tumor temperature, hyperthermia induces apoptosis, inhibits cell proliferation, and disrupts DNA repair mechanisms within GBM cells. These cellular responses play a crucial role in the therapeutic potential of hyperthermia for GBM treatment.
One particular challenge in GBM treatment is the presence of cancer stem-like cells (CSCs), a subpopulation of cells within the tumor that exhibit enhanced resistance to hyperthermia compared to other cell types. This inherent resistance contributes to treatment resistance and the recurrence of GBM tumors despite hyperthermia treatment.
Additionally, hyperthermia can activate various signaling pathways involved in cell survival, proliferation, and migration. These pathways include but are not limited to heat shock proteins and DNA damage response pathways. Activation of these pathways may have implications for the development of combination therapies that can target multiple vulnerabilities of GBM cells.
The cellular and molecular effects of hyperthermia on GBM cells provide important insights into the potential for hyperthermia as a therapeutic option. By understanding these effects, researchers and clinicians can further optimize treatment protocols to overcome treatment resistance, improve treatment outcomes, and potentially prevent tumor recurrence.
Effects of Hyperthermia on GBM Cells
| Effect | Description |
|---|---|
| Apoptosis induction | Hyperthermia triggers programmed cell death, leading to the elimination of GBM cells. |
| Cell proliferation inhibition | Elevated temperatures inhibit the ability of GBM cells to divide and proliferate, impairing tumor growth. |
| DNA repair disruption | Hyperthermia disrupts the GBM cells’ ability to repair damaged DNA, leading to genetic instability and cell death. |
| CSC resistance | Cancer stem-like cells within GBM tumors exhibit enhanced resistance to hyperthermia, contributing to treatment resistance and tumor recurrence. |
| Activation of signaling pathways | Hyperthermia activates various signaling pathways involved in cell survival, proliferation, and migration, providing opportunities for combination therapies. |
Hyperthermia Techniques for GBM Treatment
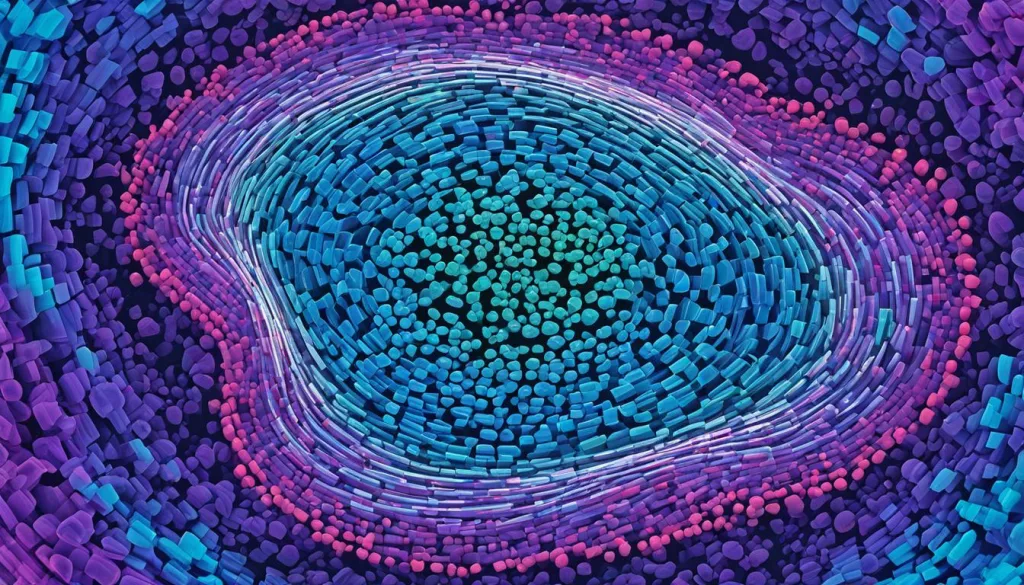
Hyperthermia, as a non-invasive treatment approach for glioblastoma multiforme (GBM), can be delivered using various techniques. These techniques include microwaves, radiofrequency, lasers, ultrasound, and magnetic fluid hyperthermia. Each technique offers unique advantages and limitations, and the selection depends on factors such as tumor location, size, and patient suitability.
The aim of these hyperthermia techniques is to raise the temperature of the tumor region, inducing tumor cell death while minimizing damage to healthy surrounding tissues.
Microwaves
Microwave hyperthermia utilizes high-frequency electromagnetic waves to heat the tumor tissue. It is commonly used in combination with other treatments, such as radiotherapy or chemotherapy, to enhance their effectiveness.
Radiofrequency
Radiofrequency hyperthermia involves applying high-frequency electrical currents to generate heat within the tumor. This technique can selectively heat the tumor while sparing adjacent healthy tissues, making it a precise therapeutic option for GBM.
Lasers
Laser hyperthermia utilizes laser light to heat the tumor tissue. The focused energy of the laser can effectively raise the tumor temperature, providing a localized treatment approach for GBM.
Ultrasound
Ultrasound hyperthermia uses high-frequency sound waves to generate heat within the tumor. It can be applied externally or internally, providing a non-invasive or minimally invasive treatment option for GBM.
Magnetic Fluid Hyperthermia
Magnetic fluid hyperthermia involves injecting magnetic nanoparticles into the tumor and applying an alternating magnetic field to generate heat. This technique offers the advantage of targeted and localized heating, minimizing damage to healthy tissues.
Image: Visualization of various hyperthermia techniques for GBM treatment.
The Impact of Hyperthermia on GBM Cells and Microenvironment
Hyperthermia not only affects GBM cells but also influences the tumor microenvironment.
During hyperthermia treatment, cells within the tumor microenvironment undergo various changes that can enhance treatment sensitivity and immunomodulation. Hyperthermia can modulate the expression of heat-shock proteins, which play a crucial role in cellular stress response. Increased expression of these proteins can lead to improved treatment outcomes by promoting apoptosis and inhibiting tumor cell growth.
Furthermore, hyperthermia can enhance antigen presentation, a vital process for the immune system to recognize and target cancer cells. By promoting the presentation of tumor-specific antigens, hyperthermia stimulates immune responses, including the activation of cytotoxic T cells and natural killer cells. This immunomodulatory effect of hyperthermia has the potential to enhance the body’s natural defense mechanisms against GBM.
In addition to its direct effects on GBM cells, hyperthermia-induced changes in the tumor microenvironment can help overcome treatment resistance. The altered microenvironment can disrupt the protective mechanisms that tumor cells use to evade therapies, making them more susceptible to other treatment modalities such as chemotherapy and radiation therapy.
Overall, hyperthermia has the potential to significantly impact both GBM cells and the tumor microenvironment, leading to improved treatment sensitivity and immunomodulation. Its ability to modulate heat-shock proteins, enhance antigen presentation, and promote immune responses makes hyperthermia a promising therapeutic approach for GBM.
Clinical Studies and Therapeutic Outcomes of Hyperthermia in GBM
Clinical studies have been conducted to evaluate the effectiveness of hyperthermia in the treatment of glioblastoma multiforme (GBM). These studies have shown promising results, indicating that hyperthermia, whether used as a standalone therapy or in combination with other treatments, can have significant therapeutic benefits for GBM patients.
1. Tumor Size Reduction
One of the key outcomes observed in clinical trials is the reduction in tumor size with hyperthermia treatment. The targeted application of heat to the tumor region can lead to the destruction of cancer cells, resulting in a decrease in tumor size. This reduction in tumor size can help alleviate symptoms, improve the patient’s overall condition, and potentially increase treatment options.
2. Improved Patient Survival
In addition to tumor size reduction, clinical studies have shown that hyperthermia can improve patient survival rates. By selectively targeting and damaging cancer cells, hyperthermia can enhance the effectiveness of traditional treatments such as surgery, radiotherapy, and chemotherapy. This combination approach may lead to improved patient outcomes and longer survival durations.
3. Enhanced Quality of Life
Patient quality of life is another important consideration in GBM treatment. Hyperthermia has demonstrated the potential to enhance the quality of life for GBM patients. By reducing tumor burden and alleviating symptoms associated with the disease, hyperthermia can significantly improve the overall well-being and functional abilities of patients. This can lead to a better quality of life, allowing them to engage in daily activities and enjoy meaningful experiences.
In summary, clinical studies have highlighted the positive therapeutic outcomes of hyperthermia in the treatment of GBM. These outcomes include tumor size reduction, improved patient survival rates, and enhanced quality of life. While the results are promising, further research is still required to optimize treatment protocols, identify suitable patient selection criteria, and evaluate the long-term effects of hyperthermia in GBM patients. Nonetheless, hyperthermia offers a potential non-invasive therapeutic option that warrants continued investigation and development.
Challenges and Limitations of Hyperthermia in GBM Treatment
Despite the potential benefits of hyperthermia in the treatment of Glioblastoma Multiforme (GBM), there are several challenges and limitations that need to be addressed. These factors play a crucial role in determining the effectiveness of hyperthermia and the overall success of GBM treatment.
Blood-Brain Barrier
One of the significant challenges in hyperthermia treatment for GBM is the blood-brain barrier (BBB). The BBB acts as a protective barrier, but it also restricts the delivery of therapeutic agents to the brain. This restricted access can limit the effectiveness of hyperthermia in reaching the tumor and hinder its therapeutic potential in GBM treatment.
Treatment Resistance
Treatment resistance is another significant challenge encountered in hyperthermia treatment for GBM. Cancer cells within the tumor can develop resistance to hyperthermia, making it difficult to achieve complete tumor eradication. This resistance is influenced by various factors, including genetic alterations, cellular heterogeneity, and the presence of cancer stem-like cells. Overcoming treatment resistance is essential to improve the efficacy of hyperthermia in GBM treatment.
Tumor Heterogeneity
Tumor heterogeneity is a critical factor that contributes to the challenges of hyperthermia treatment in GBM. GBM tumors are highly heterogeneous, consisting of diverse cell populations with different molecular characteristics and responses to treatment. This heterogeneity can lead to varying treatment responses and make it challenging to deliver effective hyperthermia treatment across all tumor regions. Precise targeting and understanding of tumor heterogeneity are necessary for successful GBM treatment.
Treatment Planning
Precise treatment planning is crucial for the effective implementation of hyperthermia in GBM treatment. The variability in tumor size, location, and patient-specific factors necessitates careful planning to ensure optimal treatment outcomes. Treatment planning involves determining the appropriate hyperthermia technique, determining the duration and intensity of treatment, and considering the integration with other treatment modalities. Advanced imaging techniques and personalized medicine approaches can aid in treatment planning and improve the efficacy of hyperthermia in GBM treatment.
Overcoming these challenges and limitations requires continuous research and technological advancements. A personalized approach that considers the individual patient’s characteristics and the specific tumor characteristics is essential to optimize hyperthermia treatment for GBM. By addressing these challenges, hyperthermia holds significant potential as a valuable therapeutic option in the comprehensive management of GBM.
Future Directions in Hyperthermia Research for GBM
As we continue to explore the potential of hyperthermia in glioblastoma multiforme (GBM) treatment, future research aims to optimize treatment protocols, develop targeted delivery strategies, and explore combination therapies to enhance treatment efficacy. By tailoring treatments to individual patients through personalized medicine approaches, taking into account factors such as patient-specific characteristics and tumor heterogeneity, we can potentially improve treatment outcomes and maximize the benefits of hyperthermia.
Advances in imaging techniques, such as real-time imaging and molecular imaging, play a crucial role in the future of hyperthermia research. These imaging technologies enable us to accurately plan and monitor the response to hyperthermia treatment. By visualizing the tumor region in real-time, we can precisely deliver hyperthermia while minimizing damage to surrounding healthy tissues. Additionally, molecular imaging allows us to assess the effectiveness of hyperthermia at the cellular level, providing valuable insights into treatment optimization and response assessment.
To further enhance the therapeutic potential of hyperthermia, combination therapies are being investigated. By integrating hyperthermia with other treatment modalities such as radiotherapy, chemotherapy, immunotherapy, or targeted therapy, we can potentially achieve synergistic effects and improve treatment outcomes. Combination therapies have the potential to overcome treatment resistance, target multiple pathways involved in GBM progression, and enhance the effectiveness of hyperthermia.
To demonstrate the potential impact of personalized medicine, combination therapies, targeted delivery, and treatment optimization on hyperthermia in GBM, let’s take a closer look at the following table:
| Treatment Approach | Advantages | Challenges |
|---|---|---|
| Personalized Medicine | – Tailored treatment based on patient-specific factors and tumor characteristics – Improved treatment outcomes – Enhanced patient satisfaction and quality of life |
– Need for comprehensive patient profiling – Access to advanced diagnostic tools |
| Combination Therapies | – Synergistic effects with hyperthermia – Overcoming treatment resistance – Targeting multiple pathways involved in GBM progression |
– Optimal sequencing and timing of therapies – Potential for increased toxicity |
| Targeted Delivery | – Precise delivery of hyperthermia to tumor region – Minimizing damage to surrounding healthy tissues |
– Overcoming the blood-brain barrier – Developing effective delivery systems and strategies |
| Treatment Optimization | – Tailoring treatment protocols to maximize efficacy – Real-time monitoring and adjustments |
– Standardizing treatment protocols – Addressing challenges specific to individual patients |
As we move forward, the combined efforts of researchers, clinicians, and technology developers hold the key to unlocking the full potential of hyperthermia in GBM treatment. Through personalized medicine, combination therapies, targeted delivery, and treatment optimization, we can strive for improved treatment outcomes, increased survival rates, and enhanced quality of life for GBM patients.
Conclusion
Hyperthermia shows promise as a non-invasive treatment approach for targeting glioblastoma multiforme (GBM). By raising the tumor temperature, hyperthermia can reduce tumor size, inhibit recurrence, and improve treatment outcomes. GBM, an aggressive and lethal brain tumor, poses significant challenges in terms of treatment efficacy and tumor recurrence. However, hyperthermia has demonstrated potential benefits in addressing these challenges.
Further research and clinical trials are needed to optimize treatment protocols and establish hyperthermia as a standard therapeutic option for GBM. Addressing the challenges and limitations of hyperthermia, such as the blood-brain barrier and tumor heterogeneity, is crucial for its successful integration into GBM treatment strategies. Additionally, the potential of hyperthermia in combination with other treatments and its impact on the tumor microenvironment require further investigation.
With ongoing advancements in personalized medicine, targeted delivery strategies, and imaging techniques, the future of hyperthermia research for GBM looks promising. By developing tailored treatment approaches and exploring combination therapies, hyperthermia could play a significant role in improving treatment outcomes for GBM patients. The long-term goal is to establish hyperthermia as a mainstream treatment option that effectively addresses tumor recurrence and enhances patient survival rates.
FAQ
What is glioblastoma multiforme?
Glioblastoma multiforme (GBM) is an aggressive and lethal brain tumor known for its high recurrence and mortality rates. It is characterized by its ability to return even after surgery, radiotherapy, and chemotherapy.
What role does hyperthermia play in GBM treatment?
Hyperthermia is a non-invasive treatment approach that involves raising the body temperature. It has shown potential benefits in reducing tumor size, inhibiting recurrence, and improving treatment outcomes in GBM patients.
How does hyperthermia affect GBM cells?
Hyperthermia induces apoptosis, inhibits cell proliferation, and disrupts DNA repair mechanisms in GBM cells. It can also influence cancer stem-like cells, which are more resistant to hyperthermia and contribute to treatment resistance and tumor recurrence.
What techniques are used to deliver hyperthermia to GBM tumors?
Hyperthermia can be delivered using various techniques such as microwaves, radiofrequency, lasers, ultrasound, and magnetic fluid hyperthermia. The choice of technique depends on factors like tumor location, size, and patient suitability.
How does hyperthermia affect the tumor microenvironment?
Hyperthermia can modulate the tumor microenvironment by influencing the expression of heat-shock proteins, enhancing antigen presentation, and stimulating immune responses. These changes can improve treatment sensitivity and enhance the effectiveness of other GBM therapies.
What do clinical studies show about the effectiveness of hyperthermia in GBM treatment?
Clinical studies have shown promising results, with hyperthermia, either alone or in combination with other treatments, associated with tumor size reduction, improved patient survival, and enhanced quality of life.
What challenges and limitations does hyperthermia face in GBM treatment?
Hyperthermia faces challenges such as the blood-brain barrier, treatment resistance, tumor heterogeneity, and the need for precise treatment planning. Overcoming these challenges requires ongoing research, technological advancements, and a personalized approach to GBM treatment.
What are future directions in hyperthermia research for GBM?
Future research aims to optimize treatment protocols, develop targeted delivery strategies, explore combination therapies, and utilize personalized medicine approaches. Advances in imaging techniques can also aid in treatment planning and response monitoring.
Can hyperthermia be considered a standard therapeutic option for GBM?
While hyperthermia shows promise, further research and clinical trials are needed to optimize treatment protocols, address challenges, and establish hyperthermia as a standard therapeutic option for GBM.