Paracentesis vs Thoracentesis — what’s the difference between these treatments?
Patients with cancer or other conditions that cause a buildup of fluids inside their abdomen or chest often need a procedure to remove that fluid.
Otherwise, that excess fluid can cause pain, breathing difficulties, or abdominal issues.
Paracentesis Explained
Paracentesis is a procedure that drains these fluids from a patient’s abdomen. Also called an abdominal tap, paracentesis is the non-toxic treatment of choice for significant abdominal fluid buildups from the following conditions:
- Severe infections of the liver or abdomen
- Various cancers
- Swelling and inflammation from other causes
- Abdominal injuries
- Cirrhosis of the liver (scarring)
- Mesothelioma
What Happens in a Paracentesis Procedure?
When you arrive at Brio-Medical, you’ll change into a hospital gown. Then our staff will help guide you into the procedure room and get onto the table. Then, they will place an intravenous (IV) catheter into a vein and attach you to equipment that monitors your vital signs.
In a paracentesis procedure, your integrative medicine provider will apply local anesthesia to your abdominal area and insert a needle into your abdomen. If needed, they might administer light sedation since it is essential to remain still during the procedure.
Sometimes, your provider might need to use ultrasound to guide the needle into place, especially if it’s difficult to locate the excess fluid. Doing so can reduce the risk of complications, as a 2013 study indicates.
Then, they will insert a catheter (a small, flexible tube) into your abdomen, allowing the fluid that has built up to drain out. After they drain all the excess fluid, they will remove the catheter and place a bandage over the puncture site. Usually, your doctor will send the fluid to a lab to learn more about any changes in your condition that might have caused the fluid buildup.
How Do I Prepare for a Paracentesis Procedure?
Before a paracentesis procedure, your provider might perform an ultrasound examination to locate the excess fluid or use other diagnostic tests to narrow down the cause of the fluid buildup. As with all-natural treatment options, it’s always best to treat the root cause of the symptoms as well as the symptoms themselves.
In addition, the provider will give you instructions about what you may eat or drink before the procedure and any traditional or holistic medicines you might need to stop taking temporarily until the procedure is over.
What Can I Expect After My Paracentesis Procedure?
First, our staff will allow you to rest while we monitor your condition. After you’ve recovered, we will help you get up. If you’ve had sedation or are lightheaded or dizzy from the procedure, you’ll need someone to drive you home.
If you have pain or discomfort, your provider will let you know which pain medication you can take. Usually, the discomfort is minimal enough that over-the-counter pain relievers are adequate for relief.
Usually, you’ll have a small amount of leakage from the procedure site. Our staff will send bandages home with you to cover the site. Be sure to keep a bandage on the site for a full 24 hours after your procedure. Don’t shower until the 24 hours have passed.
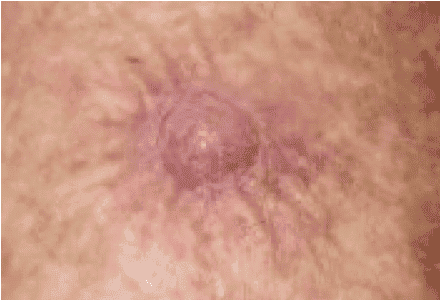
However, notify our staff if the leakage lasts longer than 24 hours after the procedure. Similarly, notify us immediately if you develop redness at the procedure site, a fever, increased abdominal pain, chills or shaking, difficulty breathing, or heavy leakage.
Thoracentesis Explained
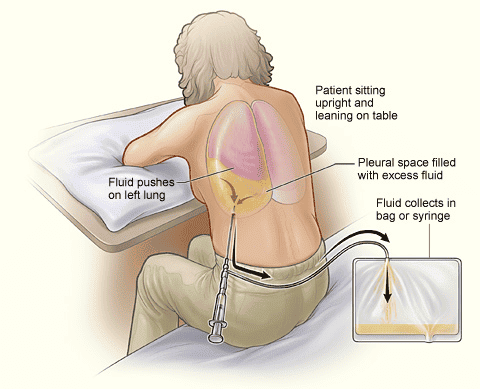
Similar to paracentesis, thoracentesis removes excess fluid from the body. However, thoracentesis removes fluid from the pleural space surrounding a patient’s lungs, not their abdomen. Unlike paracentesis, doctors use thoracentesis to remove excess air and fluid from the lungs.
When fluid builds up in the pleural space, the lungs can’t fully inflate, causing shortness of breath and even pain. Thoracentesis can help relieve that discomfort and restore normal breathing function.
Doctors use thoracentesis to diagnose and treat the symptoms of the following conditions:
- Congestive heart failure (CHF)
- Cancer, especially of the lungs
- Lung infections
- Autoimmune diseases, such as systemic lupus erythematosus (SLE)
- Pancreatitis
- Pulmonary embolisms (blood clots in the lung)
- Empyema (a buildup of pus in the pleural space)
- Tuberculosis (TB)
- Pneumonia
- Liver failure
- Chest injuries
What Happens in a Thoracentesis Procedure?
As with many treatments, you’ll change into a hospital gown after arrival at Brio-Medical’s Scottsdale location. Our staff will help prepare you for the procedure, including inserting an IV catheter in case you need hydration or other medications.
Although sedation usually isn’t necessary, our team can provide it if you are anxious or have difficulty remaining still. If you do have sedation, bring someone with you who can drive you home. Finally, the staff will hook you up to equipment to monitor your vitals and provide you with oxygen, either a face mask or a nasal tube.
Usually, doctors perform the procedure with you sitting, with your arms positioned on a table above the bed to open the spaces between your ribs. Then, they’ll inject you with a local anesthetic deep in the skin and muscle tissue surrounding the area.
After the surrounding area is numb, the doctor will insert a needle between your ribs to draw out the excess fluid or air. In some cases, they will use ultrasound to guide the needle or find areas of excess fluid, as a 2022 paper on thoracentesis advises.
During the procedure, the doctor might ask you to hold your breath or breathe out deeply, depending on the situation. Otherwise, try to remain still.
For large amounts of fluid, the doctor will use a catheter instead of a needle, draining the fluid into a bag. Often, they will send the fluid to a lab for testing. Afterward, the doctor might take a chest X-ray to ensure your lungs are completely clear.
After the doctor finishes the procedure, they will apply a bandage to absorb any leakage and protect the site from infection. Be sure not to remove it for 24 hours.
How Do I Prepare for a Thoracentesis Procedure?
Ask your doctor if they have any requirements about refraining from eating, drinking, or taking certain medications — especially if you’re taking blood thinners. Be sure to notify your doctor about all your medicines, including over-the-counter and holistic therapies.
Ask your doctor about any concerns you might have about the procedure. Also, let our staff know if you’re pregnant, have any other health conditions you’ve not disclosed, or are allergic to any medications, as well as latex or tape.
What Can I Expect After My Thoracentesis Procedure?
While you’re still at the clinic, the staff will check your vital signs and the puncture site for any excessive leakage or bleeding. The procedure is only minimally invasive, so you should not experience much pain or discomfort afterward. Your provider will advise you on which medications you can take to alleviate any post-procedure discomfort.
After you have recovered from the procedure, we’ll send you home. Usually, it’s best to arrange for someone to drive you home.
Avoid bathing or showering for 24 hours when you arrive home to ensure adequate healing. Avoid strenuous activities for a few days.
In most cases, patients experience few post-procedure complications. However, be sure to call our clinic if you experience:
- A fever of 100.4 degrees or more
- Excessive swelling or redness at the procedure site
- Blood or excessive fluid leaking from the procedure site
- Shortness of breath or chest pain
- Or any other symptoms that hamper your daily activities
If you have a condition that requires paracentesis or thoracentesis, you can rest assured that our staff will make your experience as free of discomfort as possible. To learn more about Brio-Medical’s broad range of integrative treatments for cancer and other illnesses, schedule your free consultation today!
Schedule My Consultation (button)
Paracentesis vs Thoracentesis - References
“About Your Paracentesis (Abdominal Tap).” Memorial Sloan Kettering, https://www.mskcc.org/cancer-care/patient-education/paracentesis-abdominal-tap. Accessed August 24, 2022.
“Paracentesis.” Penn Medicine, https://www.pennmedicine.org/-/media/documents%20and%20audio/patient%20forms/interventional%20radiology/paracentesis.ashx. Accessed August 24, 2022.
Mercaldi, Catherine J, and Stephan F Lanes. “Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and paracentesis.” Chest vol. 143,2 (2013): 532-538. doi:10.1378/chest.12-0447
“Thoracentesis.” Johns Hopkins Medicine, https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/thoracentesis. Accessed August 24, 2022.
Wiederhold BD, et al. “Thoracentesis.” StatPearls (2022).
“Thoracentesis.” Michigan Medicine, https://www.med.umich.edu/1libr/pulmonary/Thoracentesis.pdf. Accessed August 24, 2022.