The following article covers the differences between cancer tumor cells vs cancer stem cells.
Cancer has remained an enigma for centuries, with countless researchers dedicating their entire careers to figuring out this phenomenon. On the bright side, years of study have yielded effective treatments, including natural remedies, for the various types of cancer.
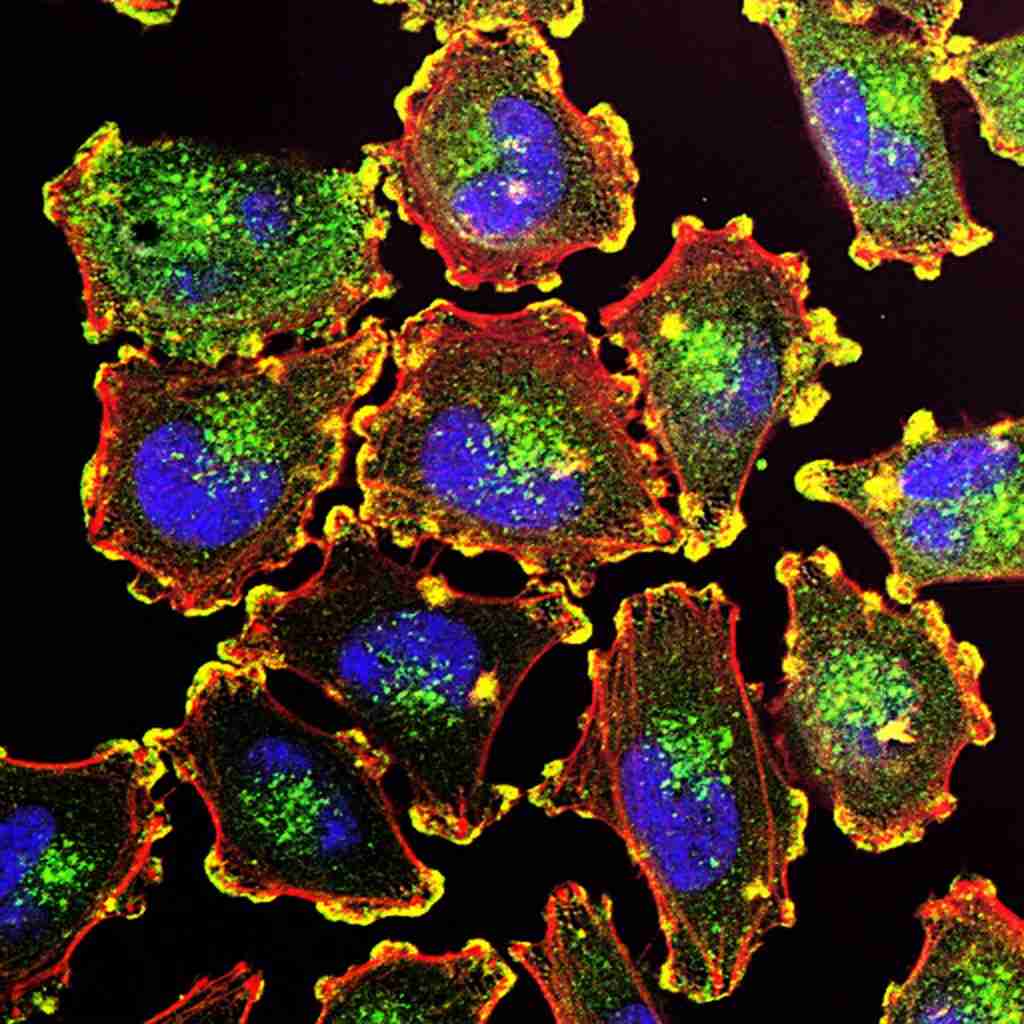
So far, it’s become clear that the key to understanding cancer is to investigate the disease at its most basic — the cellular level where it all begins. Neoplastic cells are morphologically and physiologically diverse from normal healthy cells. These differences help to uncover the secrets of cancer and develop highly targeted anticancer treatments.
This article gives a basic overview of what researchers have gathered about the two main types of neoplastic cells: cancer tumor cells and cancer stem cells.
But in order to understand the characteristics and physiology of tumor cancer cells and cancer stem cells, it’s important to have some basic knowledge of the cell cycle.
Cell Cycle and the Root of Cancer
The average adult body is made up of an estimated 30 trillion cells. But this figure represents only a minuscule fraction of all the cells produced in an average human lifespan. As cells age and die, they are continuously replaced and replenished by new ones at a rate of about 330 billion cells every day. This happens through cell division, which is tightly regulated by the mechanisms of the cell cycle.
The cell cycle is divided into four phases:
- G1 Phase – The cell prepares for DNA replication.
- S (Synthesis) Phase – DNA is replicated.
- G2 Phase – The cell prepares for division.
- M (Mitosis) Phase – The parent cell divides into two daughter cells. The daughter cells can re-enter the G1 Phase immediately if further replication is required. Otherwise, they go into a temporary or irreversible resting phase (G0). This fate is determined by growth factors.
The process of cell division is prone to errors. But multiple checkpoints in the cell cycle preserve genome integrity by ensuring that genetic errors are not passed on to the daughter cells. At the end of the G1 Phase, a checkpoint examines the cell for DNA damage and may halt the cycle to repair any detected damage. The G2 checkpoint assesses the cell for incomplete or erroneous DNA replication. If a defect is detected at this stage, the checkpoint may trigger programmed cell death (apoptosis). During mitosis, another crucial checkpoint sees that the replicated genes are correctly distributed in both daughter cells.
These checkpoints and the entire cell cycle are regulated by proteins called cyclins, which are, in turn, controlled by proteins such as retinoblastoma and p53. But even with these checkpoints in place, some DNA or genetic errors do make it to the daughter cells. Over time, one or more cells can accumulate enough genetic errors or “mutations” to become neoplastic. Cancerous cells are abnormal cells that essentially take on a life of their own, defying critical physiological functions and regulations. They override the cell cycle mechanisms and continue to divide regardless of DNA damage and the absence of cycling and growth signals.
Here are the common hallmarks of cancer cells:
- Require little to no growth factors to proliferate
- Unspecialized or undifferentiated
- Genetically unstable or corrupted
- Physically deformed
- Resistant to apoptosis
- Divide infinitely
- Trick the immune system into sparing them
- Evade growth suppressors
- Often clump together to form tumors
- Stimulate blood vessels to grow around them for sustenance (angiogenesis)
- Can metastasize (spread to other tissues and organs)
Cancer Tumor Cells vs Cancer Stem Cells
Most cancers, apart from blood cancers such as leukemia, form tumors. A tumor is a lumpy mass of tissue made up of abnormal or neoplastic cells. Every tumor starts off microscopically small and can take several months or even years to grow just a few millimeters in size. But the tumor eventually grows big enough to compromise the health and functions of the surrounding tissues or the host organ.
There are two types of tumors: malignant and benign. Malignant tumors can spread to other tissues or organs, while benign tumors remain at the site of formation.
It was long thought that tumor cells were homogeneous, but recent research shows that tumors comprise various types of cells, mainly cancer tumor cells and cancer stem cells (CSC).
Cancer formation involves a series of random mutations that can occur in any gene. The uncontrolled activation of proto-oncogenes or deactivation of tumor suppressor genes can lead to tumor formation. Also, some of the mutations can affect the genes associated with cell division mechanisms. Cells with such mutations often acquire the stem cell ability to divide rapidly. These are known as cancer stem cells. They can seed and grow a tumor by endlessly cloning themselves. The duplicates become either new CSCs or cancer tumor cells.
Cancer stem cells only make up a small portion of a cancerous tumor. But multiple lab and animal studies show that CSCs are critical drivers of cancer tumor growth, angiogenesis, and metastasis. In some cases, CSCs transplanted in mice test subjects were found to seed cancerous tumors in their new hosts. Many oncologists believe that this phenomenon could be the reason for cancer recurrence after successful tumor removal or treatment.
In fact, most chemotherapy drugs target cells exhibiting stem-like behavior such as rapid mitosis. Unfortunately, such drugs might not reach the cancer stem cells at a tumor’s core, meaning they can only kill so many cells before the treatment plateaus. Another downside to treating cancer this way is that the drugs indiscriminately attack healthy rapidly-dividing cells such as those found in hair roots. This is the reason chemo medications cause hair loss.
Given that CSCs were discovered fairly recently, more research is needed to clearly understand the role of cancer stem cells in tumor formation and growth and how their characteristics may be reverseengineered to fight cancer.
Cancer Tumor Cells vs Cancer Stem Cells – Conclusion
Although it’s not all in black and white, cancer research has come a long way in the last few decades. Thanks to new scientific findings and theories, such as the discovery of CSCs, the oncological world is teeming with promising New Age cancer treatments. Cancer patients now have a vast selection of traditional and alternative anticancer solutions.
Brio-Medical offers a wide range of natural holistic remedies that heal the body as well as the mind and soul. Reach out to learn more about personalized holistic treatments for cancer and other chronic diseases.
References:
- Baba AI, Câtoi C. “Chapter 3, TUMOR CELL MORPHOLOGY.” Comparative Oncology. Bucharest (RO): The Publishing House of the Romanian Academy (2007).
- Fischetti, Mark, and Jen Christiansen. ”Our Bodies Replace Billions of Cells Every Day.” Scientific American, April 1, 2021. Accessed: August 23, 2022.
- OpenStax Biology. “The cell cycle.” (CC BY 3.0). Accessed August 23, 2022.
- Khan Academy. “Cell cycle regulators.” Accessed August 23, 2022.
- Levine, Michelle S, and Andrew J Holland. “The impact of mitotic errors on cell proliferation and tumorigenesis.” Genes & development vol. 32,9-10 (2018): 620-638. doi:10.1101/gad.314351.118
- Yu, Zuoren et al. “Cancer stem cells.” The international journal of biochemistry & cell biology vol. 44,12 (2012): 2144-51. doi:10.1016/j.biocel.2012.08.022.
- National Cancer Institute. “What Is Cancer?” Understanding Cancer. Updated: May 5, 2021. Accessed August 23, 2022.
- Ayob, A.Z., Ramasamy, T.S. “Cancer stem cells as key drivers of tumor progression.” J Biomed Sci 25, 20 (2018). Accessed August 23, 2022.